Coverage of Nonpharmacologic Treatments for Low Back Pain Among US Public and Private Insurers
SOURCE: JAMA Netw Open. 2018 (Oct 5); 1 (6): e183044
James Heyward, MPH; Christopher M. Jones, PharmD, MPH; Wilson M. Compton, MD, MPE; et al
Center for Drug Safety and Effectiveness,
Johns Hopkins Bloomberg School of Public Health,
Baltimore, Maryland.
IMPORTANCE: Despite epidemic rates of addiction and death from prescription opioids in the United States, suggesting the importance of providing alternatives to opioids in the treatment of pain, little is known regarding how payers’ coverage policies may facilitate or impede access to such treatments.
OBJECTIVE: To examine coverage policies for 5 nonpharmacologic approaches commonly used to treat acute or chronic low back pain among commercial and Medicare Advantage insurance plans, plus an additional 6 treatments among Medicaid plans.
DESIGN, SETTING, AND PARTICIPANTS: Cross-sectional study of 15 commercial, 15 Medicaid, and 15 Medicare Advantage health plans for the 2017 calendar year in 16 states representing more than half of the US population. Interviews were conducted with 43 senior medical and pharmacy health plan executives from representative plans.
MAIN OUTCOMES AND MEASURES: Medical necessity and coverage status for the treatments examined, as well as the use of utilization management tools and cost-sharing magnitude and structure.
RESULTS: Commercial and Medicare insurers consistently regarded physical and occupational therapy as medically necessary, but policies varied for other therapies examined.
Payers most commonly covered
physical therapy (98% [44 of 45 plans]),
occupational therapy (96% [43 of 45 plans]), and
chiropractic care (89% [40 of 45 plans]),
while transcutaneous electrical nerve stimulation (67% [10 of 15 plans]) and steroid injections (60% [9 of 15 plans]) were the most commonly covered among the therapies examined for Medicaid plans only.
Despite evidence in the literature to support use of acupuncture and psychological interventions, these therapies were either not covered by plans examined (67% of all plans [30 of 45] did not cover acupuncture) or lacked information about coverage (80% of Medicaid plans [12 of 15] lacked information about coverage of psychological interventions). Utilization management tools, such as prior authorization, were common, but criteria varied greatly with respect to which conditions and what quantity and duration of services were covered. Interviewees represented 6 Medicaid managed care organizations, 2 Medicare Advantage or Part D plans, 9 commercial plans, and 3 trade organizations (eg, Blue Cross Blue Shield Association). Interviews with plan executives indicated a low level of integration between the coverage decision-making processes for pharmacologic and nonpharmacologic therapies for chronic pain.
There are more articles like this @ our:
CONCLUSIONS AND RELEVANCE: Wide variation in coverage of nonpharmacologic treatments for low back pain may be driven by the absence of best practices, the administrative complexities of developing and revising coverage policies, and payers’ economic incentives. Such variation suggests an important opportunity to improve the accessibility of services, reduce opioid use, and ultimately improve the quality of care for individuals with chronic, noncancer pain while alleviating the burden of opioid addiction and overdose.
From the FULL TEXT Article:
Introduction
Opioid overdose deaths in the United States have risen to epidemic proportions, driven by an approximate 4–fold increase in prescription opioid sales that occurred between 1999 and 2010. [1, 2] While deaths from heroin and highly potent synthetic opioids such as illicit fentanyl have increased dramatically since 2010, prescription opioids remain a major contributor to overdose deaths in the United States. In 2016, 42,249 people died from overdoses due to prescription or illicit opioids in the United States, with 17,087 deaths attributed to prescription opioids [3, 4] and more than 2 million individuals estimated to have a prescription opioid use disorder. [5] Projections suggest that an even greater number of Americans will be found to have died from an opioid overdose in 2017. [6]
Although many factors have contributed to increased use of opioids during the past 2 decades, 1 important contributor has been their overuse for the treatment of chronic, noncancer pain in the absence of data demonstrating long-term benefit. [7–9] This is important because opioids are but 1 of many pharmacologic and nonpharmacologic treatments for pain from chronic conditions such as lower back pain, headache, and fibromyalgia. In 2016, the Centers for Disease Control and Prevention released its Guideline for Prescribing Opioids for Chronic Pain, [10] recommending the use of nonopioid and nonpharmacologic therapies as first-line treatment for chronic pain. Consistent with other recent clinical practice guidelines, [11–13] the Centers for Disease Control and Prevention also advises that if opioids are prescribed, they should be combined with nonpharmacologic and nonopioid therapies. An increasing volume of evidence and consensus demonstrates the role of many of these approaches in clinical practice, underscoring the opportunities that exist to simultaneously improve the quality of care for those with pain while reducing exposure to and overreliance on prescription opioids. [14–17]
Recognizing the importance of nonopioid therapies, the US Department of Health and Human Services’ National Pain Strategy urges changes to insurers’ coverage policies to enable greater access and adherence to nonopioid therapies for pain. [9] Although coverage policies are an important determinant of health services utilization, little is known regarding payers’ coverage of nonpharmacologic treatments for chronic, noncancer pain. This information gap constrains the policy development and implementation process.
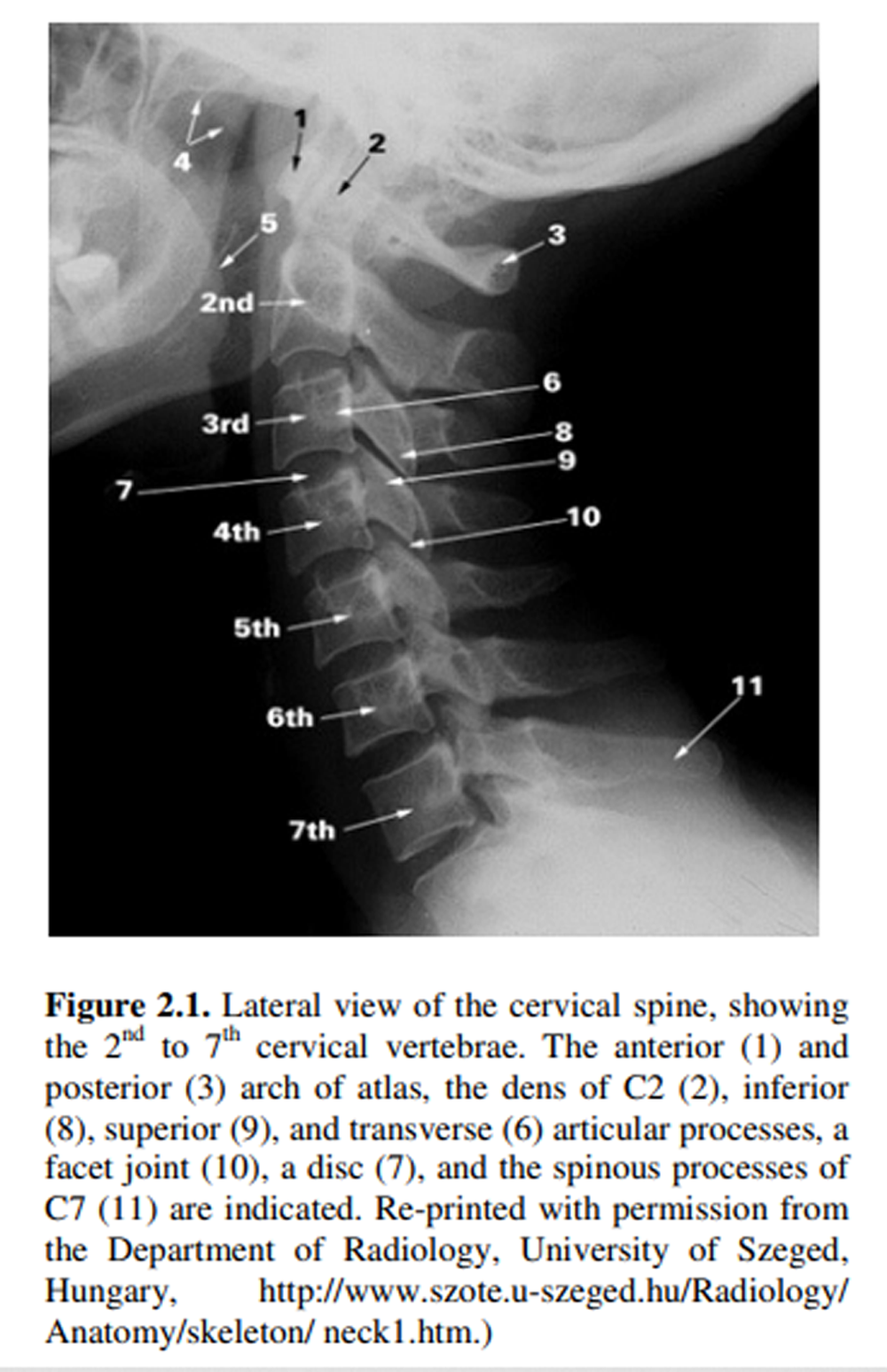
To address this gap, we examined 2017 policies for these treatment modalities for low back pain — 1 of the most common pain-related conditions — among a diverse sample of 45 commercial, Medicaid, and Medicare Advantage plans. We focused on 5 common nonpharmacologic therapies for pain across all plans (physical therapy, occupational therapy, chiropractic care, acupuncture, and therapeutic massage), and, owing to the greater availability of information in public Medicaid coverage documents, examined an additional 6 therapies among Medicaid plans (transcutaneous electrical nerve stimulation [TENS], psychological interventions, steroid injections, facet injections, laminectomy, and diskectomy). We also conducted key informant interviews with 43 senior executives from the examined plans to better understand how plans have determined coverage and utilization management criteria for the treatments of interest. The aim of the study was to describe the current landscape of coverage for these therapies, and we did not conduct any formal hypothesis testing or infer causal pathways regarding coverage policies among the sampled plans.
Read the rest of this Full Text article now!




Leave A Comment