Identification Of Subgroups Of Inflammatory And Degenerative MRI Findings In The Spine And Sacroiliac Joints: A Latent Class Analysis Of 1037 Patients With Persistent Low Back Pain
SOURCE: Arthritis Res Ther. 2016 (Oct 13); 18 (1): 237
Bodil Arnbak, Rikke Krüger Jensen, Claus Manniche,
Oliver Hendricks, Peter Kent, Anne Grethe Jurik
and Tue Secher Jensen
Research Department,
Spine Centre of Southern Denmark,
Hospital Lillebaelt,
Oestre Hougvej 55, Middelfart, 5500, Denmark.
bodil.arnbak@rsyd.dk
BACKGROUND:   The aim of this study was to investigate subgroups of magnetic resonance imaging (MRI) findings for the spine and sacroiliac joints (SIJs) using latent class analysis (LCA), and to investigate whether these subgroups differ in their demographic and clinical characteristics.
METHODS:   The sample included 1037 patients aged 18—40 years with persistent low back pain (LBP). LCA was applied to MRI findings of the spine and SIJs. The resulting subgroups were tested for differences in self-reported demographic and clinical characteristics.
RESULTS:   A five-class model was identified: Subgroup 1, ‘No or few findings’ (n = 116); Subgroup 2, ‘Mild spinal degeneration’ (n = 540); Subgroup 3, ‘Moderate to severe spinal degeneration’ (n = 229); Subgroup 4, ‘Moderate to severe spinal degeneration with mild SIJ findings’ (n = 68); and Subgroup 5, ‘Mild spinal degeneration with moderate to severe SIJ findings’ (n = 84). The two SIJ subgroups (Subgroups 4 and 5) had a higher median activity limitation score (Roland Morris Disability Questionnaire calculated as a proportional score: 65 (IQR 48—78)/65 (48—78)) compared with Subgroups 1—3 (48 (35—74)/57 (39—74)/57 (39—74)), a higher prevalence of women (68% (95% CI 56—79)/68% (58—78)) compared with Subgroups 2 and 3 (51% (47—55)/40% (33—46)), a higher prevalence of being overweight (67% (95% CI 55—79)/53% (41—65)) compared with Subgroup 1 (36% (26—46)) and a higher prevalence of previous LBP episodes (yes/no: 81% (95% CI 71—91)/79% (70—89)) compared with Subgroup 1 (58% (48—67)). Subgroup 5 was younger than Subgroup 4 (median age 29 years (IQR 25—33) versus 34 years (30—37)) and had a higher prevalence of HLA—B27 (40% (95% CI 29—50)) compared with the other subgroups (Subgroups 1—4: 12% (6—18)/7% (5—10)/6% (3—9)/12% (4—20)). Across the subgroups with predominantly spinal findings (Subgroups 1—3), median age, prevalence of men, being overweight and previous LBP episodes were statistically significantly lower in Subgroup 1, higher in Subgroup 2 and highest in Subgroup 3.
There are more articles like this @ our:
CONCLUSIONS:   Five distinct subgroups of MRI findings in the spine and SIJs were identified. The results indicate that SIJ MRI findings not only can be seen as a part of the spondyloarthritis disease entity, but also are associated with age, gender and being overweight. Furthermore, the results indicate that LBP patients with SIJ MRI findings are more disabled compared with patients without SIJ MRI findings, and that moderate to severe spinal degeneration and/or SIJ MRI findings may be associated with recurrent pain.
KEYWORDS:   Cluster analysis; Low back pain; Magnetic resonance imaging; Sacroiliac joints; Spine; Spondyloarthritis
From the FULL TEXT Article:
Background
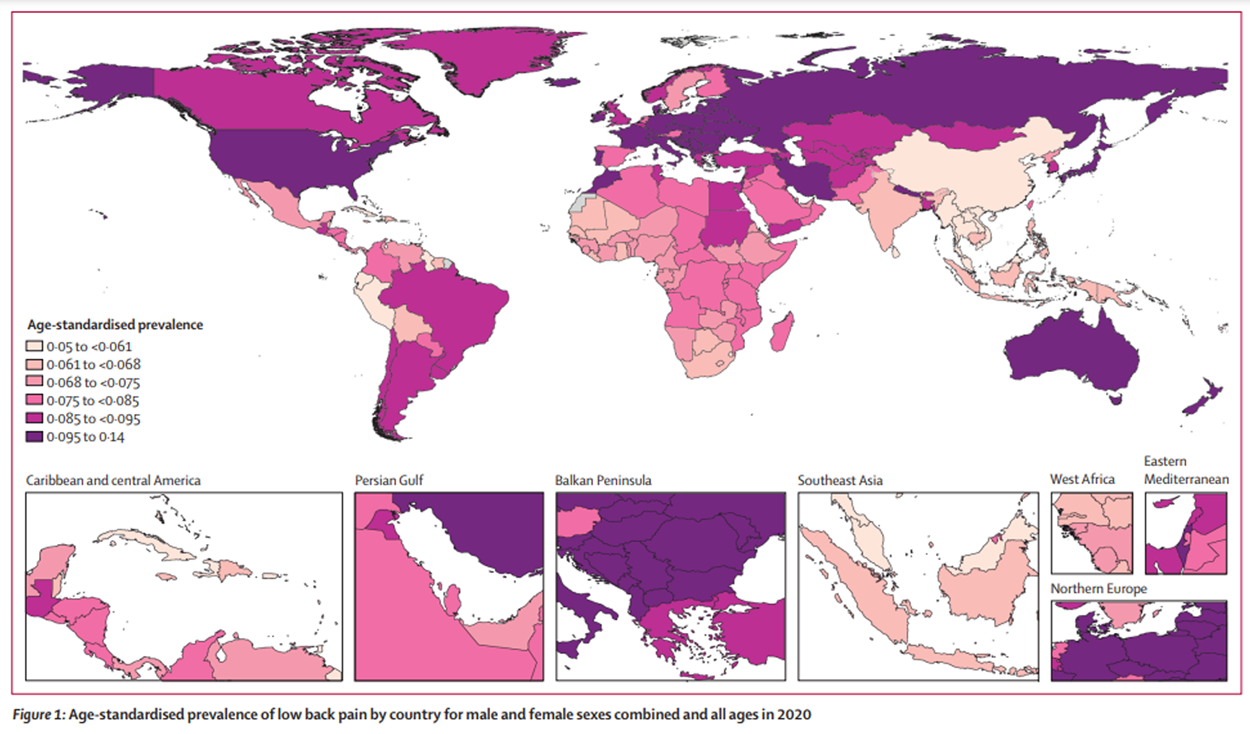
Low back pain (LBP) is a serious and disabling health condition that is estimated to be the number—one cause of years lived with disability. [1] More knowledge about the various causes of LBP is needed to improve diagnosis and treatment. The use of magnetic resonance imaging (MRI) has increased dramatically in recent decades in an attempt to optimise the diagnostic process for persistent LBP and spondyloarthritis (SpA). Nevertheless, many uncertainties remain about the association between MRI findings and the clinical presentation of back pain. [2—5]
Several MRI findings, including degenerative findings such as disc degeneration, disc herniations and vertebral endplate signal changes (i.e. Modic changes), have been associated with clinical presence of LBP. Also, and findings at the sacroiliac joints (SIJs) (i.e. sacroiliitis) have been associated with the clinical diagnosis of SpA. However, the strength of these associations is often reported to be relatively weak. [2—5] This might be because previous studies have focused on individual MRI findings [2—5], even though multiple MRI findings with varying severity are often present at the same time. In a recent cross—sectional population study of over 1,000 people, some degree of lumbar disc degeneration was present in the majority of the population. [6] Although the presence of disc degeneration was only weakly associated with LBP, the association with LBP increased with the severity of disc degeneration across disc levels. [6] Likewise, the severity of MRI finding at the SIJs defining a ‘SpA positive MRI’ is reported to influence the diagnostic value. [7] Focusing on the presence of individual MRI findings may therefore oversimplify the complexity of the degenerative and inflammatory axial processes and the interactions between various MRI findings, with the risk of overlooking potentially important clinical information.
In studies of MRI findings and LBP, there has been a focus on spinal degenerative MRI findings, while the SIJs have traditionally been the focus for studies of SpA. Recent research, however, indicates that MRI findings at the SIJs, previously thought to be indicative of SpA, are prevalent in patients with non—specific LBP. [ 7, 8] Also, spinal MRI findings associated with SpA can be difficult to distinguish from common degenerative vertebral endplate signal changes, which complicate the assessment of SpA. [9] Further to this, degenerative and SpA—related MRI research findings are most often reported in separate studies and in different study populations, which potentially reduces their applicability to daily clinical practice. There is therefore a need to explore the co—existence of degenerative and SpA—related MRI findings in both the spine and SIJs and their association with the clinical presentation of LBP. There may also be more than one pattern of co—existent MRI findings (subgroups), each of which has a different association with LBP.
Latent class analysis (LCA) is a multivariable statistical technique that attempts to find the subgroup structure which maximises the between—subgroup variance and minimises the within—subgroup variance, as a means to best explain the overall variance in the data. LCA has a number of advantages over traditional statistical clustering techniques, including greater classification accuracy, more precise metrics of subgroup model performance, the provision of posterior probabilities for subgroups and for individuals in each subgroup as a measure of subgroup model certainty, and the ability to manage variables of all data types (dichotomous, ordinal and continuous). [10, 11] This novel statistical method therefore offers the possibility to explore patterns of MRI findings with the potential of identifying clinically important subgroups.
Read the rest of this Full Text article now!



Leave A Comment