DCs Treating the Multiple Sclerosis Patient
SOURCE: ACA News ~ May 2015 ~ FULL TEXT
By Lori A. Burkhart
Multiple Sclerosis (MS) is the most common disabling neurological disease of young adults, according to the National Institutes of Health (NIH), most often appearing when people are between 20 and 40 years old. However, it can also affect children and adults over 40. The U.S. National Library of Medicine defines MS as an autoimmune disease that affects the central nervous system (brain and spinal cord). The myelin sheath, a protective membrane that wraps around the axon of a nerve cell, is destroyed in a patient with MS; this is caused by inflammation. That damage causes nerve signals to slow down or stop. MS affects women more than men.
Since doctors of chiropractic are recognized as primary contact neuromusculoskeletal specialists, most will have patients with undiagnosed MS come into their practices. The DC will diagnose the patient, treat certain symptoms and make the appropriate referrals.
Diagnosis
Diagnosis of MS is complicated in that it can be severe or mild and can go into remission. NIH points out that initial symptoms often are double or blurred vision, red-green color distortion or blindness in one eye. Most MS patients experience muscle weakness in their extremities and difficulty with coordination and balance.
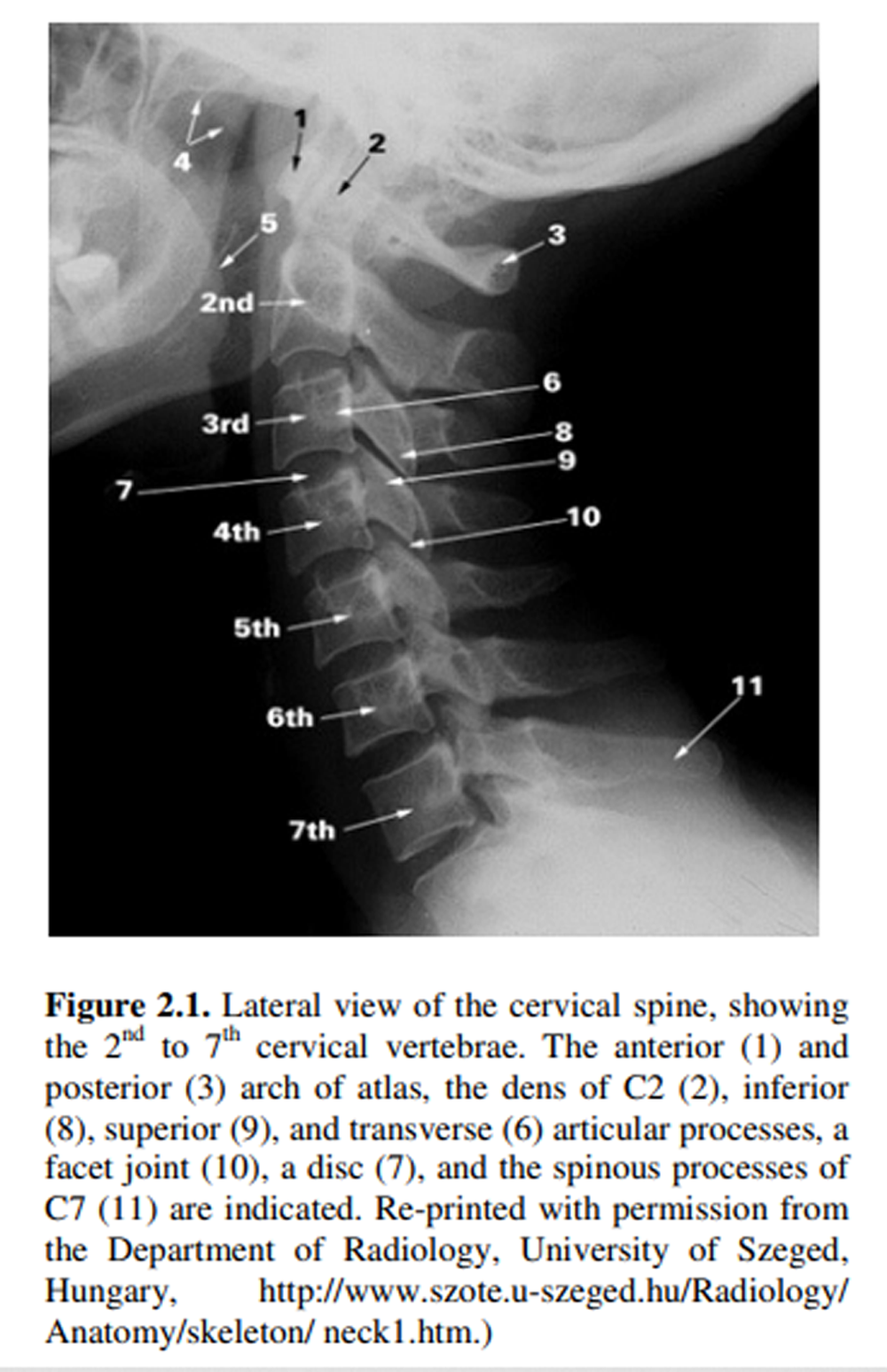
According to Larry Wyatt, DC, DACBR, FICC, professor and senior faculty, division of clinical sciences at Texas Chiropractic College, MS is diagnosed in a number of ways, as its clinical course is distinctive in each patient and there are different types of MS. Some patients with obvious MS are diagnosed by clinical signs and symptoms (i.e., attacks) alone. These patients will have MS attacks that often relapse for months or even years. In other patients further testing is necessary. Magnetic resonance imaging (MRI), often with gadolinium enhancement, is the mainstay of diagnosis in most cases. “Patients with MS will very often have multiple high-signal intensity lesions in the brain and/or spinal cord on T2-weighted images,” Dr. Wyatt says. “In addition, cerebrospinal fluid analysis for immunoglobulin content can be quite helpful. There is a specific set of criteria, called the McDonald Criteria, which outline the findings necessary for the diagnosis of the different forms of MS.”
Jason West, DC, DCBCN, a fourth-generation DC who operates a clinic in Pocatello, Idaho, says the majority of the diagnosis comes from the patient history, but he points out that usually when patients with MS come in, they already are diagnosed and they are unhappy with their medical treatment options. “If they weren’t diagnosed, one of the standards is to do an MRI and look for white lesions, and there is also a spinal tap to look for antibodies,” Dr. West says. “Usually these patients have a history of peripheral neuropathy or neurological disease or processes occurring.”
Symptom Management
There is no cure for MS. There is only management of symptoms, and MDs typically treat with medications such as corticosteroids and interferon. In most cases there is a natural, although unpredictable, course of remissions and exacerbations. Dr. Wyatt points out that this can make it difficult to ascertain the effectiveness of any therapeutic regimen. “From the perspective of the chiropractic physician, treatment is focused on the management of the neuromusculoskeletal sequelae of the disease,” he says. “Manual therapies and rehabilitation can be quite helpful in managing those sequelae, but there is no evidence to support the idea that such therapies will alter the course of the disease. Therapeutic exercise seems to show the most promise. Nutritional therapy has not been shown to alter the course of the disease.”
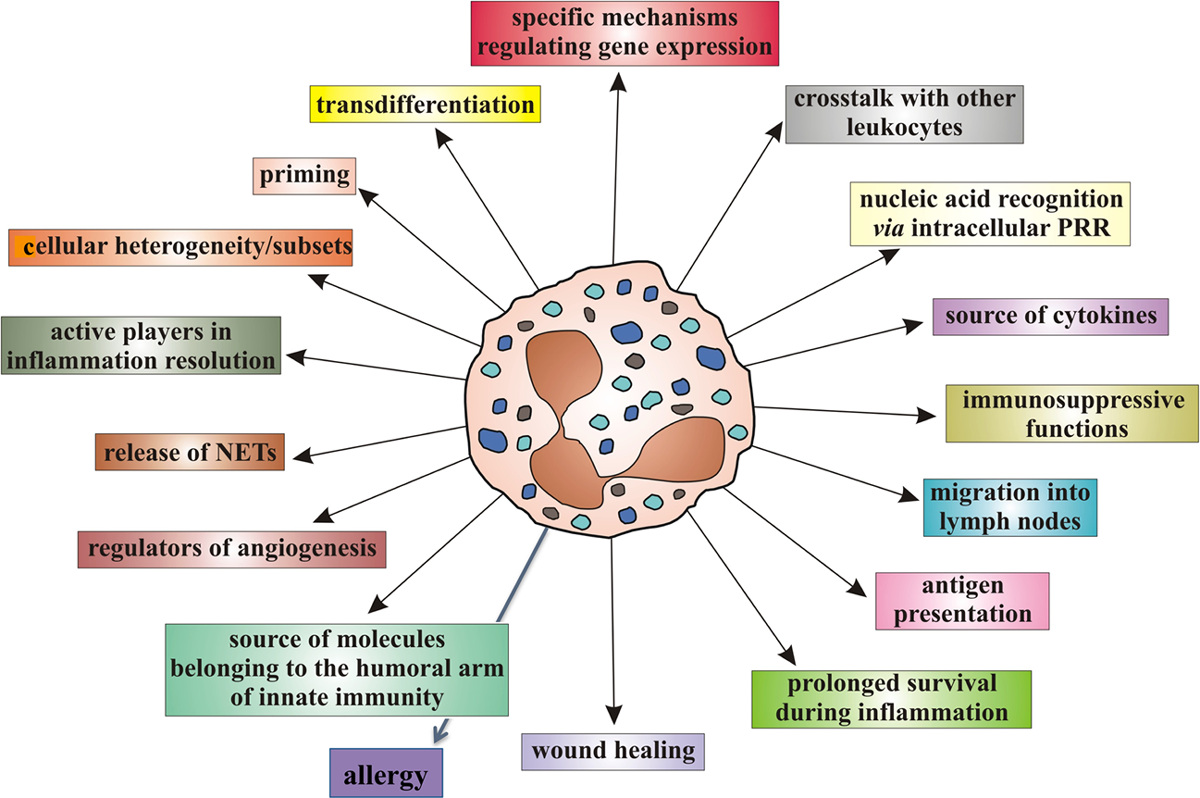
“Neuromusculoskeletal adjustments are one way to balance the body, and those are palliative to patients with MS,” Dr. West says. He thinks of MS as a dysfunctional immune disease and says, “The worse thing we can do is give immunosuppressant therapy that knocks down the immune system.” He continues, “Perhaps the medical treatment is working for some people, but I usually have people come in to my office who say, ‘I’ve been put on Enbrel or Humera or methotrexate, and I feel awful.’” He adds that these patients are actively looking for treatment options. “I am not anti-medicine, and in some cases, patients need short-term anti-inflammatories,” he says. “As a profession, we do a fantastic job on MS if the DC has the confidence to treat it, especially because we treat nerves.”
From an overall wellness perspective, Dr. West tells patients not to abuse their bodies, to eat well and to have the right environment. He points out that there are a lot of emotional problems associated with chronic diseases. “I tell patients whether it’s prayer, meditation, emotional release or counseling, you have to deal with the emotions. I am hands-off on how they do that, but it is something they need to do.”
Generally, Drs. Wyatt and West are unaware of any definitive contraindications to manual therapy for MS specifically, save for those contraindications that would apply to all patients. But Dr. Wyatt cautions, “That being said, the use of modalities in patients with MS who experience sensory losses may be contraindicated, as the patient would be unable to voice any adverse reactions as they wouldn’t be able to feel the sensations associated with such reactions. As to manipulation, the general rules of contraindications would apply.”
Read the rest of this Full Text article now!



Leave A Comment