Manual Treatment For Cervicogenic Headache And Active Trigger Point In The Sternocleidomastoid Muscle: A Pilot Randomized Clinical Trial
J Manipulative Physiol Ther. 2013 (Sep); 36 (7): 403—411
Gema Bodes-Pardo, PT, MSc, Daniel Pecos-Martín, PT, PhD, Tomás Gallego-Izquierdo, PT, PhD, Jaime Salom-Moreno, PT, MSc, César Fernández-de-las-Peñas, PT, PhD, Ricardo Ortega-Santiago, PT, PhD
Clínica Fisioterapia Santiago Vila,
San Fernando de Henares, Spain.
OBJECTIVE: The purpose of this preliminary study was to determine feasibility of a clinical trial to measure the effects of manual therapy on sternocleidomastoid active trigger points (TrPs) in patients with cervicogenic headache (CeH).
METHODS: Twenty patients, 7 males and 13 females (mean ± SD age, 39 ± 13 years), with a clinical diagnosis of CeH and active TrPs in the sternocleidomastoid muscle were randomly divided into 2 groups. One group received TrP therapy (manual pressure applied to taut bands and passive stretching), and the other group received simulated TrP therapy (after TrP localization no additional pressure was added, and inclusion of longitudinal stroking but no additional stretching). The primary outcome was headache intensity (numeric pain scale) based on the headaches experienced in the preceding week. Secondary outcomes included neck pain intensity, cervical range of motion (CROM), pressure pain thresholds (PPT) over the upper cervical spine joints and deep cervical flexors motor performance. Outcomes were captured at baseline and 1 week after the treatment.
There’s a lot more material like this @ our:
Headache and Chiropractic Page and the:
RESULTS: Patients receiving TrP therapy showed greater reduction in headache and neck pain intensity than those receiving the simulation (P < .001). Patients receiving the TrP therapy experienced greater improvements in motor performance of the deep cervical flexors, active CROM, and PPT (all, P < .001) than those receiving the simulation. Between-groups effect sizes were large (all, standardized mean difference, >0.84).
CONCLUSION: This study provides preliminary evidence that a trial of this nature is feasible. The preliminary findings show that manual therapy targeted to active TrPs in the sternocleidomastoid muscle may be effective for reducing headache and neck pain intensity and increasing motor performance of the deep cervical flexors, PPT, and active CROM in individuals with CeH showing active TrPs in this muscle. Studies including greater sample sizes and examining long-term effects are needed.
From the FULL TEXT Article:
Introduction
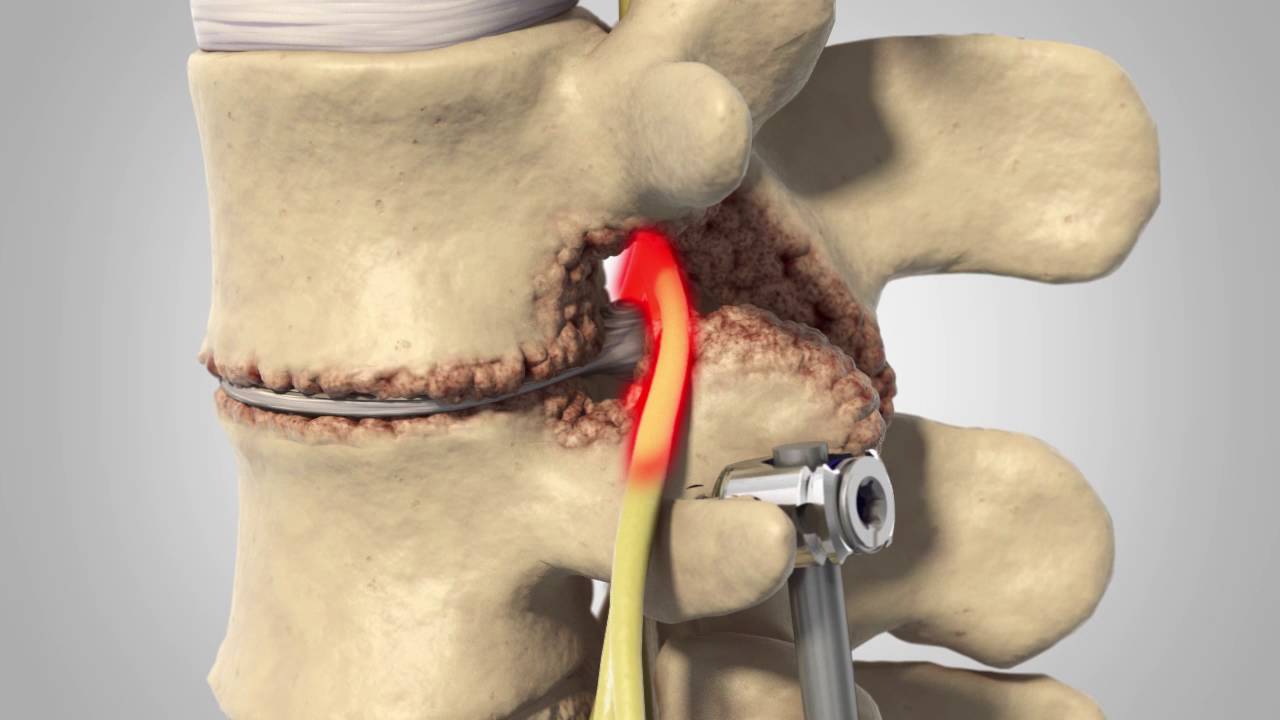
Cervicogenic headache (CeH) is a secondary headache, which means “head pain with a cervical source.” [1, 2, 3] It is characterized by unilateral headache with symptoms and signs of neck involvement, for example, pain by movement, by external pressure over the upper cervical, and/or sustained awkward head positions. [2, 3] Prevalence rates for CeH varied in the general population because some studies have not detailed the criteria used to define the headache. Prevalence rates within the general population varied from 0.4% to 2.5%, [4, 5] with a female preponderance (2:1). [6] However, Sjaastad and Bakketeig [7] reported a prevalence of 4.1% with no female preponderance.
Physical therapy is commonly used for the management of individuals with CeH. [8] Previous systematic reviews reported preliminary evidence for the application of upper cervical spine mobilization or mobilization for the management of CeH. [9, 10, 11] A recent systematic review of manual therapies suggests that spinal manipulative might be an effective treatment in the management of CeH patients. [12] A survey study conducted in Australia revealed that upper cervical spine mobilization or manipulation was the most used intervention by physical therapists. [13] The physiologic basis of CeH pain lies in the convergence between trigeminal afferents and afferents from the upper cervical spinal nerves in the trigeminocervical nucleus caudalis. [14, 15] Nociceptive afferent inputs into trigeminocervical nucleus may be originated by spondylosis, disk lesions, or facet arthropathies in the upper cervical spine. [16, 17] Therefore, therapeutic interventions targeted to tissues innervated by the trigeminocervical nucleus caudalis can be effective for the management of individuals with CeH.
Read the rest of this Full Text article now!



Leave A Comment