Bulletproof Your Documentation
SOURCE: Chiropractic Economics
By Kathy Mills Chang
Part 1: Ensure your admitting and ongoing paperwork isn’t slipping through the cracks
Because of the many different techniques and philosophies involved in chiropractic, you can be assured different doctors utilize different admitting and ongoing paperwork.
A recent survey of 80 chiropractors revealed that 72 percent of them collected paperwork for their clinic from various sources, creating a patchwork effect. Because very few utilized an actual system of paperwork, they admitted concern that some documentation could fall through the cracks.
So, what paperwork should you have in your office?
History
Most state chiropractic boards that have a standard of care for patients include taking patient history. If one were to follow the evaluation and management documentation guidelines, history is a significant portion of the value.
Because the requirements entail collecting information about the chief complaint; the history of the present illness; a review of systems; and the patient’s past, family, and social history, there is a substantial amount of information that can and should come from the patient.
Having information laid out in a clear fashion on your admitting paperwork allows the patient to answer the majority of the essential initial consultation questions. Using your admitting paperwork as a template allows you to ensure the required bullet points will be answered by the patient and reviewed by the physician.
There are many more articles like this @ our:
A simple review of the evaluation and management requirements for the history section should allow you to compare your existing initial paperwork to be ideal. Make sure you have ample space available within your questions to make physician notes, as these become part of your permanent record.
Some doctors prefer to have a separate consultation sheet to review this information. Others prefer to have space available within the patient history to save time and create efficiency in the consultation process.
Guidelines for the requirement of initial patient history can be found in the Center for Medicare and Medicaid Services (CMS) Evaluation and Management Documentation Guidelines, your state board of chiropractic examiners documentation rules, or medical review policy from individual insurance carriers you participate with.
In order to ensure your history meets all of the requirements, gather all of these and compare your initial admitting and follow-up paperwork to be sure yours pass muster.
Additionally, many doctors hoping to improve their documentation and recordkeeping choose to include in the history questions related to the patient’s activities of daily living deficits. When selecting functional goals in your treatment plan, this information is invaluable.
Examination
The clinical examination is the doctor’s opportunity to expand upon objective findings discovered in the initial or follow-up visits. Your examination form should be complete with all major tests expected to meet the standard of care required in your examination.
A thorough understanding of the CMS Evaluation and Management Guidelines assists in knowing minimum requirements for the various levels of coding used in the office.
While it is important to list all possible tests that could be performed, remember that a form listing every test in the chiropractic profession could cause problems should you find yourself on the witness stand or in an audit.
If you elect not to perform a particular orthopedic or neurological test on the list on the patient, you must indicate on your record, “Not performed,” or, N. P. — then you must prepare yourself to be asked why you elected not to perform that test.
Because periodic follow-up examinations performed within the same round of episodic care require the doctor to repeat positive tests from the first exam, it’s often helpful to have subsequent examinations listed on the same form. This makes it easy to review your initial exam and follow up what is necessary at the periodic re-evaluation.
However, should the patient return for care for a new episode, it would be prudent to utilize your initial exam form again and start from scratch.
If you feel you need a review of the most common orthopedic and neurological tests performed, the book, “Practical Assessment of the Chiropractic Patient,” by K. Jeffrey Miller, DC, DABCO, is recommended.
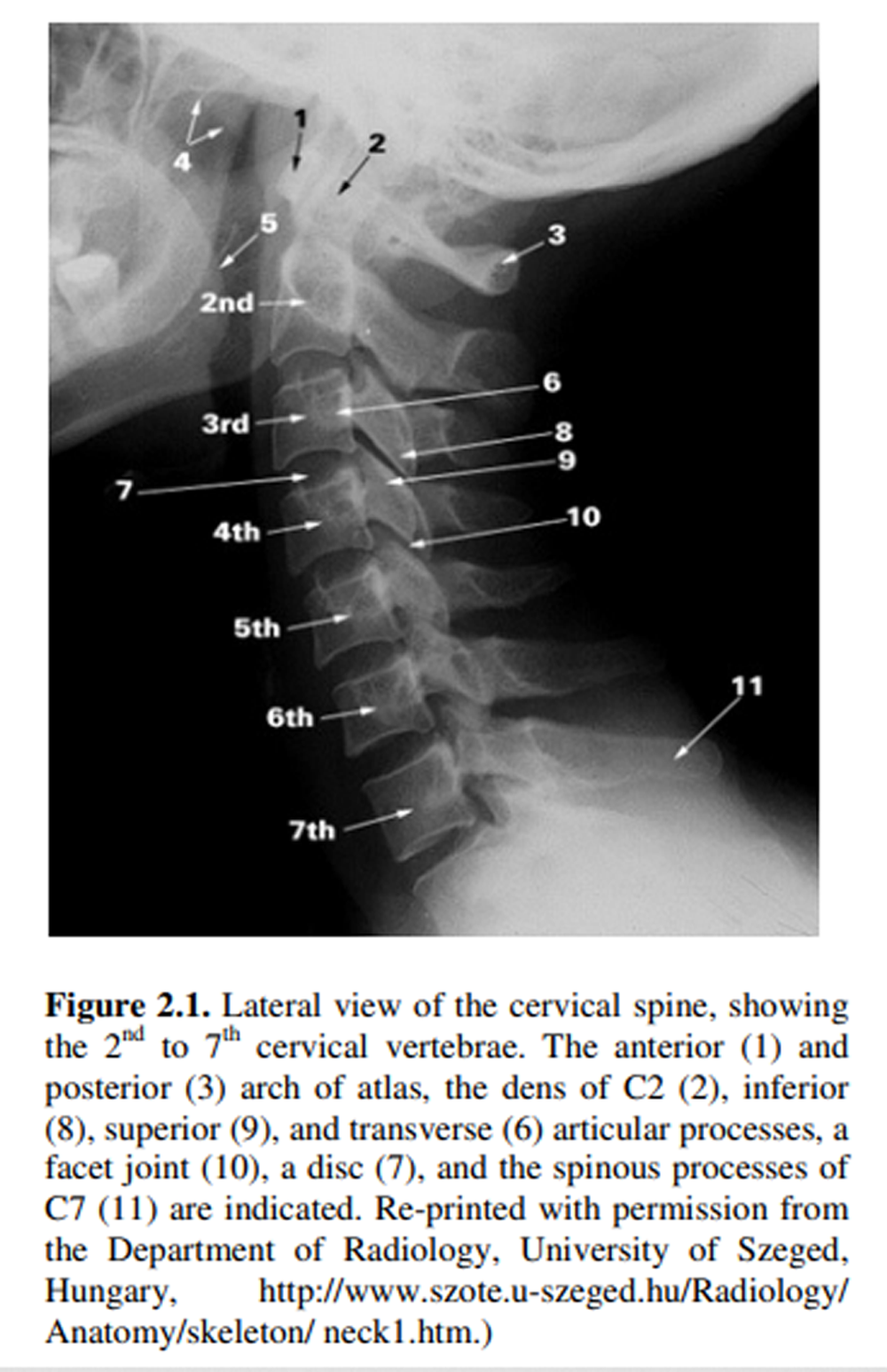
Or, you can review Richard C. Schafer, DC, PhD’s
Orthopedic and Neurologic Procedures in Chiropractic
right here, right now!
The CMS Evaluation and Management Guidelines layout an explanation of what is expected in the examination portion of your evaluation and management service. These guidelines indicate the recognized body systems that should be included in the exam as well as the recognized body areas.
For example: It is often a surprise to chiropractors that the six body areas recognized are listed as follows: head and neck; spine, ribs, and pelvis; right upper extremity; left upper extremity; right lower extremity; and left lower extremity.
Based on a typical examination that would include the head, neck, spine, ribs, and pelvis, a doctor would only have met the requirement for two body areas. This may be far more limiting to your ability to code appropriately than you may realize. Be sure you collect the evaluation and management guidelines and compare with your existing examination form.
Remember, this examination carries tremendous weight in establishing medical necessity. Therefore, make sure your form meets all of the requirements.
Diagnosis
There are many ways doctors choose to list the diagnosis that is part of the treatment record. The diagnosis goes along with the entire treatment episode so it’s important to list all of the appropriate diagnosis codes.
If the doctor chooses to include massage in the plan, a muscle-related diagnosis is necessary. Likewise, disc-related treatment should be warranted by a disc diagnosis code.
One of the easiest ways to accomplish this, not only to make it easy on the doctors, but also creating ease for the staff, is to have a master diagnosis sheet. This diagnosis sheet would contain all of the potential diagnosis codes you would typically use and be available as part of the record.
Ideally, these diagnosis codes would be divided and categorized. For example: Muscle-related diagnosis codes, disc-related diagnosis codes, and other tissue-specific diagnoses would be grouped together.
It’s important to review all of the diagnosis codes you use on a periodic basis. Because changes occur almost every year, it’s also important to get a diagnosis reference manual and update your form periodically.
The beauty of having a diagnosis sheet is they can become part of the record and be placed together with other paperwork grouped by episode of care. In a paperwork system, these various forms, including the diagnosis sheet, could be color-coded. That way, the beginning, middle, and end of an episode could be obvious in your patient’s chart.
Remember, just because you hand the diagnosis codes to your team to enter into your practice management software, does not mean the patient’s record contains the diagnosis, which is a requirement. Use of a diagnosis sheet alleviates these concerns.
This review is only effective if you use it to compare it with what you already have. If you feel your paperwork could use a tune up, there are many options.
For example: Many practice management companies have put together systems of paperwork. Companies, such as Parker Share, have paperwork available for purchase. You can also check out www.newpatientpaperwork.com to read about a complete paper documentation system now available for doctors in the profession.
The remaining paperwork necessary to bulletproof your documentation includes the treatment plan, functional daily notes, the re-evaluation, and the discharge.
Treatment plan
Read the rest of this article at our:



Leave A Comment