Chiropractic Research & Practice State of the Art
SOURCE: Cleveland Chiropractic College
By Daniel Redwood, D.C., professor,
Cleveland Chiropractic College
Peer Reviewers: Carl S. Cleveland III, D.C., J.
Michael Flynn, D.C., Cheryl Hawk, D.C., PhD., and
Anthony Rosner, PhD.
©2010 Cleveland Chiropractic College –
Kansas City and Los Angeles
Chiropractic Research & Practice
State of the Art
Since chiropractic’s breakthrough decade in the 1970s — when the U.S. federal government included chiropractic services in Medicare and federal workers’ compensation coverage, approved the Council on Chiropractic Education (CCE) as the accrediting body for chiropractic colleges, and sponsored a National Institutes of Health (NIH) conference on the research status of spinal manipulation — the profession has grown and matured into an essential part of the nation’s healthcare system.
Chiropractic was born in the United States in the late 19th century and the U.S. is home to approximately 65,000 of the world’s 90,000 chiropractors. [1] The chiropractic profession is the third largest independent health profession in the Western world, after medicine and dentistry. Doctors of chiropractic are licensed throughout the English-speaking world and in many other nations as primary contact providers, licensed for both diagnosis and treatment without medical referral. In 2005, the World Health Organization (WHO) published WHO Guidelines on Basic Training and Safety in Chiropractic, which documented the status of chiropractic education and practice worldwide and sought to ensure high standards in nations where chiropractic is in the early stages of development. [2]
Rigorous educational standards are supervised by government-recognized accrediting agencies in many nations, including CCE in the United States. After fulfilling college science prerequisites similar to those required to enter medical schools, chiropractic students must complete a chiropractic college program of four academic years, which includes a wide range of courses in anatomy, physiology, pathology, and diagnosis, as well as spinal adjusting, physiotherapy, rehabilitation, public health and nutrition.
The NIH classifies chiropractic as a manipulation and body-based form of complementary and alternative medicine (CAM), although chiropractors, mindful of the major strides they have made toward mainstream status, often prefer to be known as “integrative” rather than CAM practitioners. [3] Utilization rates for both chiropractic and CAM are substantial.
Chiropractors in the United States see approximately 19 million individual patients per year. At least one third of U.S. adults routinely use CAM therapies, and Americans schedule hundreds of millions of office visits per year to licensed CAM professionals, at a cost of tens of billions of dollars. [4]
Chiropractic shares with other CAM professions a health philosophy that emphasizes the inherent recuperative and self-healing capacities of the body, with a worldview based on promoting balance of body and mind through natural methods of prevention and treatment. Chiropractic is the only profession identified as CAM whose services are covered by a substantial majority of health insurance policies.
Research: Cornerstone of Professional Development
In the years since the 1970s, research on the effectiveness of chiropractic care, particularly the manual methods described as spinal manipulation or adjustment (94% of which is delivered by chiropractors), [5] has expanded considerably. There are now approximately 100 randomized clinical trials on spinal manipulation. Most of these involve investigations into its effects on back pain, neck pain, and headaches, but a growing number of projects address other areas of chiropractic practice, including extremity (leg and arm) problems and nonmusculoskeletal conditions such as infantile colic and hypertension. In a large majority of these studies, spinal manipulation outperformed comparison therapies or placebo. Significantly, not a single patient in any of these studies experienced a major adverse side-effect.
To strengthen the chiropractic research community, the U.S. Health Resources and Services Administration funded for 12 years (1995–2006) an annual chiropractic Research Agenda Conference (RAC), where researchers and practitioners met to hear reports on completed studies, propose and implement new research projects, develop strategies for interdisciplinary collaboration, and advance the overall direction of chiropractic research. After the completion of this seed funding from the federal government, the profession has self-funded continued annual RAC meetings in conjunction with the annual meeting of the Association of Chiropractic Colleges.
The resulting upsurge in chiropractic research has been dramatic. As Scott Haldeman, DC, MD, PhD, who presided over the World Health Organization’s Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders, wrote in 2010, “There was a time, not long ago, when there was little or no evidence to support the practice of manipulation that is the mainstay of chiropractic practice … There has, however, been a rapid growth in the number of clinical trials that have studied the effectiveness of manipulation, mobilization and massage over the past 20 years and … there is now little dispute amongst knowledgeable scientists that manipulation is of value in the management of back pain, neck pain and headaches that make up 90% or more of all patients who seek chiropractic care.” [6]
Most of the research cited below focuses on the effectiveness of manual adjustment (manipulation) of the spine and other musculoskeletal structures. While this is the chiropractor’s primary area of specialty, the care delivered by chiropractors includes much more, reflecting chiropractors’ expertise in diagnosis, radiology, rehabilitation, physiotherapy, non-manipulation manual methods (mobilization and massage), nutrition, prevention, and health promotion, along with their widely acknowledged skills in doctor-patient relationships. [7, 8] In a 1998 Archives of Internal Medicine article, Harvard Medical School professors Kaptchuk and Eisenberg described these relationships appreciatively: “Chiropractic’s ultimate lesson may be to reinforce the principle that the patient-physician relationship is fundamentally about words and deeds of connection and compassion. Chiropractic has managed to embody this message in the gift of the hands.” [8]
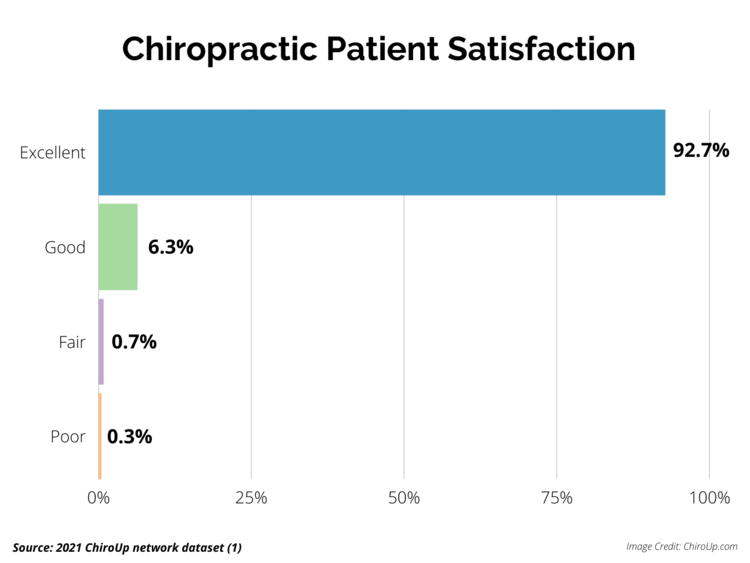
Patient satisfaction with chiropractic care is based on many factors, foremost among these the judgment by patients that their therapeutic goals — particularly relief of pain and restoration of function — have been met or exceeded. In 2010, the Secretary of Health and Human Services, Kathleen Sebelius, submitted a Report to Congress on the Demonstration of Coverage of Chiropractic Services Under Medicare. [9] This report noted that, “Sixty percent of respondents indicated that they received ‘complete’ or ‘a lot’ of relief of symptoms from their chiropractic treatments.
Satisfaction with care was high, with 87 percent reporting levels of 8 or higher on a 10-point scale and 56 percent indicating a perfect score of 10. Similarly high proportions reported that chiropractors listened carefully and spent sufficient time with them.”
Low Back Pain
Read the rest of this Full Text article now!


Thanks for sharing this long, detailed and informative post. Keep posting!