Acupuncture and Chiropractic Care for Chronic Pain
in an Integrated Health Plan: A Mixed Methods Study
SOURCE: BMC Complement Altern Med. 2011 (Nov 25); 11 (1): 118
DeBar LL, Elder C, Ritenbaugh C, Aickin M, Deyo R, Meenan R, Dickerson J, Webster JA, Jo Yarborough B.
Kaiser Permanente, The Center for Health Research, Portland, Oregon, USA. lynn.debar@kpchr.org
BACKGROUND: Substantial recent research examines the efficacy of many types of complementary and alternative (CAM) therapies. However, outcomes associated with the “real-world” use of CAM has been largely overlooked, despite calls for CAM therapies to be studied in the manner in which they are practiced. Americans seek CAM treatments far more often for chronic musculoskeletal pain (CMP) than for any other condition. Among CAM treatments for CMP, acupuncture and chiropractic (A/C) care are among those with the highest acceptance by physician groups and the best evidence to support their use. Further, recent alarming increases in delivery of opioid treatment and surgical interventions for chronic pain–despite their high costs, potential adverse effects, and modest efficacy–suggests the need to evaluate real world outcomes associated with promising non-pharmacological/non-surgical CAM treatments for CMP, which are often well accepted by patients and increasingly used in the community.
METHODS: This multi-phase, mixed methods study will: (1) conduct a retrospective study using information from electronic medical records (EMRs) of a large HMO to identify unique clusters of patients with CMP (e.g., those with differing demographics, histories of pain condition, use of allopathic and CAM health services, and comorbidity profiles) that may be associated with different propensities for A/C utilization and/or differential outcomes associated with such care; (2) use qualitative interviews to explore allopathic providers’ recommendations for A/C and patients’ decisions to pursue and retain CAM care; and (3) prospectively evaluate health services/costs and broader clinical and functional outcomes associated with the receipt of A/C relative to carefully matched comparison participants receiving traditional CMP services. Sensitivity analyses will compare methods relying solely on EMR-derived data versus analyses supplementing EMR data with conventionally collected patient and clinician data.
DISCUSSION:
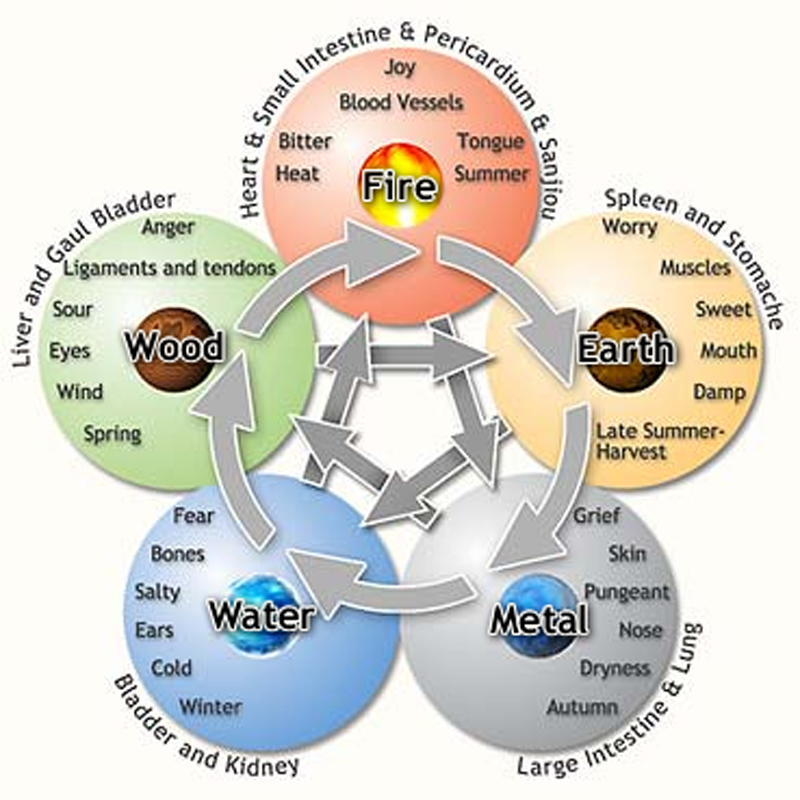
We expect that successful completion of this study will provide an evaluation of the outcomes—from the perspectives of patients, providers, and health services utilization—associated with the real-world use of A/C services. By comparing the results of the EMR-only analyses with the more comprehensive results available in Phase 3, we will be able to identify the strengths and weaknesses of EMR-alone analyses and potentially identify the most critical additional data needed. We further anticipate that the trio of EMR-based analyses, qualitative assessment, and prospective cohort studies will provide a clearer understanding of the decisionmaking processes behind the use of A/C for CMP; these will also provide a transportable methodology that can be applied to other health care settings, CAM treatments, and clinical populations. With regard to advancing our understanding of patients’ use of CAM in everyday practice settings, much CAM research to date has focused narrowly on “early adopters” (those likely to use CAM services regardless of barriers[117]). Yet within our cohort, cost and access barriers are substantially reduced, allowing us to study other factors (see Figure 1) influencing A/C care receipt and outcomes and to develop a comprehensive characterization of A/C use patterns and outcomes in patients with increasing access to such CAM services. An important goal of this study is to clarify how CMP patients use A/C compared to conventional care (to augment or replace it), when and why patients disclose A/C use to allopathic providers, and how such practices may vary by patient characteristics. Our mixed methods approach will help us develop a better understanding of the process behind the decision to initiate (patients), recommend (allopathic providers), and continue (patients and providers) A/C care for the treatment of CMP. Finally, studying this in everyday treatment settings allows us to consider the range of services received in A/C care (e.g., needling or spinal manipulation vs. whole systems-based care) and variation by characteristics of the CMP patient and/or A/C provider.
In addition to advancing our understanding of real world A/C practices and their impact on CMP, this study affords us the opportunity to build upon the increasingly available EMR systems to conduct research that may be more broadly adopted to better understand the real world interplay of conventional medicine and A/C services. Using EMRs exclusively may limit information on important variables (covariates) on which to match or cluster like patients. However, by augmenting data sets through direct reports by providers and patients regarding important decision-making factors suggested by qualitative findings, we may substantially reduce potential confounding in comparing those who do and do not receive A/C treatment. Thus, we can identify whether widely available data in EMR and administrative systems can be used to adequately forecast patients’ outcomes and evaluate the extent to which supplementation from additional patient- and provider-collected information is a necessary adjunct to EMR-based data analysis.
Finally, our MCG-focused methodology gives us a unique opportunity to conduct patientcentered research; that is, to identify like groups based upon actual individual patient care characteristics rather than hypothetical group averages. A typical RCT may not include enough participants to form homogeneous clusters for separate evaluation, yet an EMR database of a large clinical population like the CMP sample described here does include sufficient numbers of patients with similar characteristics and disease severity to form clinically meaningful clusters as the basis of the analyses. Accordingly, this research may allow us to address the clinical question as follows: for whom does supplementary CAM care result in clinically significant improvements in pain severity and overall functioning? Our planned MCG methodology will allow us to identify the characteristics of CMP patients for whom A/C may have the greatest impact on satisfaction, functioning, clinical, and QOL outcomes; it will also clarify whether the timing of services relative to conventional care and the course of the CMP affects such outcomes.

Another great article! I had several of my employees read this and then passed it on! Our clinic thanks you! Great Job
Having used both chiropractic and acupuncture methods
for overe 35 years I find them to be highly effective together.
They seem in the majority of cases to be better used togtter than by themselves.
A knowledge and use of microacupunctue systems as well as soft tissue and cranial techniques also enhanances both traditional acupuncture and chiropractic methods
Hello. Great job. I did not expect this on a week day. This is a great story. Thanks!